Reframing the Definition of Obesity
Sabina Paglialunga, PhD Senior Director, Scientific Affairs
Two notable guidance documents addressing obesity and weight loss were issued in January 2025. Surprisingly, they have differing opinions on the role body mass index (BMI) plays in the definition of obesity and the clinical management of patients with obesity.
The two documents in question are:
- The Lancet Diabetes & Endocrinology Commission: Definition and diagnostic criteria of clinical obesity
- Food and Drug Administration (FDA): Obesity and Overweight: Developing Drugs and Biological Products for Weight Reduction Guidance for Industry
The recent FDA guidance defines obesity as a chronic disease characterized by excess adiposity and recommends using BMI, an anthropometric index, to classify weight groups. BMI is calculated as:
BMI = weight (kg) / [height (m)]2
The formula has been around since the 1800’s. It was developed by Adolphe Quetelet, a Belgian statistician, mathematician, and astronomer, in 1832. However, it wasn’t validated as a measure of obesity until the 1970s by physiologist Ancel Keys (reviewed in Pray & Riskin). Now, BMI is commonly applied to assess health and stratify disease risk. BMI cutoff values are applied to classify overweight (25-29.9 kg/m2) and obesity class 1 (30-34.9 kg/m2), obesity class 2 (35-39.9 kg/m2) and extreme obesity (≥40 kg/m2).
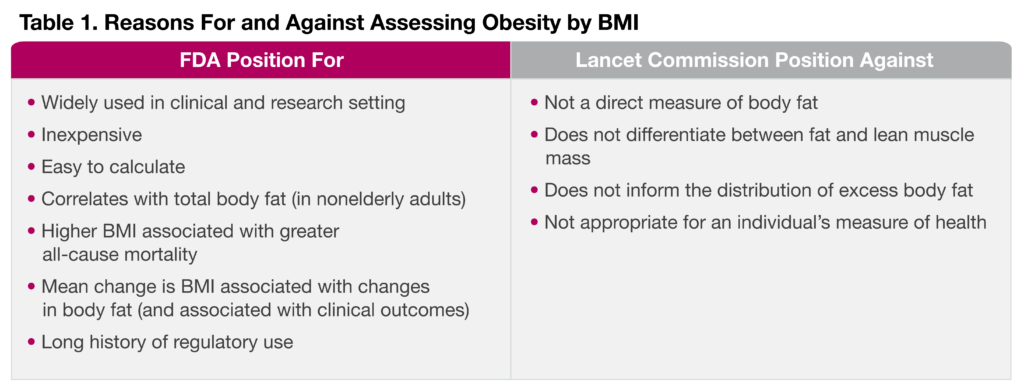
Weighing the Utility of BMI
While BMI is a convenient and long-standing measure to assess obesity, it does not differentiate between fat and lean muscle mass. It can either under- or over-estimate adiposity (fat mass). For example, older adults, conditions associated with bone or muscle mass loss, and certain ethnicities are prone to underestimation of obesity and fat mass by BMI, while conversely athletes could have overestimated obesity rates. Therefore, the Lancet Commission recommends that excess adiposity should be confirmed by either of the following as a second measure of fat mass, in addition to BMI:
- Waist circumference
- Waist-to-hip ratio
- Waist-to-height ratio
- Bioimpedance
- Direct measures of body fat such as dual X-ray absorptiometry (DEXA) or magnetic resonance imaging (MRI)
One exception, however, is that clinicians may assume that a patient with a BMI ≥40 kg/m2 displays excess adiposity. The arguments to utilize or limit BMI in determining obesity are as follows.
Redefining Obesity
More poignant, the Lancet report also provides an updated and evidence-based definition of obesity, applying clinical and biological criteria for the diagnosis of this chronic illness.
- Clinical obesity: a chronic, systemic illness characterized by alterations in the function of tissues, organs, the entire individual, or a combination thereof due to excess adiposity. Clinical obesity can lead to severe end-organ damage, causing life-altering and potentially life-threatening complications (e.g., heart attack, stroke, and renal failure).
- Preclinical obesity: a state of excess adiposity with preserved function of other tissues and organs and a varying, but generally increased, risk of developing clinical obesity and several other non-communicable diseases (e.g., type 2 diabetes, cardiovascular disease, certain types of cancer, and mental disorders).
The aim of reframing the definition of obesity and its assessment is to encourage more accessibility and effective management for those with an unmet need. Until recently, obesity alone, without the presence of other diseases, was not considered a disease in itself (reviewed in Rubino et al.). This potentially led to negative implications for treatment options and insurance coverage for those with excess body fat without other comorbidities. However, relying on BMI alone with these new definitions could lead to overdiagnosis of obesity, therefore direct excess fat assessment in addition to physical work-up is recommended.
Conclusion
While these two reports may seem at odds with each other, the Lancet Commission does concede that BMI should be used only as a surrogate measure of health risk at a population level, for epidemiological studies, or screening purposes. The latter is most notable for drug developers. Therefore, in line with the FDA guidance, BMI will continue to be the main inclusion criteria for weight loss clinical trials. However, additional markers of excess fat could provide better insight into drug effects on adiposity. To that end, Celerion has extensive experience with weight reduction drugs, including GLP-1 receptor agonists, insulin-sensitizing drugs, and microbiota products. We also offer a full range of adiposity assessments, including BMI, body weight, waist circumference, and bioimpedance, as well as sophisticated imaging assessments such as DEXA, MRI, and FibroScan® (liver fat content).
Reference
FDA. Obesity and Overweight: Developing Drugs and Biological Products for Weight Reduction Guidance for Industry. 2025. https://www.fda.gov/media/71252/download
Pray R, Riskin S. The History and Faults of the Body Mass Index and Where to Look Next: A Literature Review. Cureus. 2023 Nov 3;15(11):e48230. DOI: 10.7759/cureus.48230
Rubino F et al. Redefining obesity: advancing care for better lives. The Lancet Diabetes & Endocrinology. 2025 Jan 14;13(2):75. DOI: 10.1016/S2213-8587(25)00004-X
